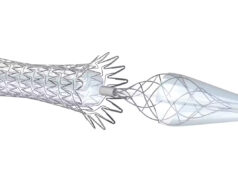
The international CREST-2 study has found that, for people with severe carotid artery narrowing who have not experienced recent stroke symptoms, a minimally invasive carotid artery stenting (CAS) procedure—combined with intensive medical therapy—significantly lowered stroke risk compared with medical therapy alone. The more traditional surgical approach of carotid endarterectomy (CEA) did not show the same benefit, however.
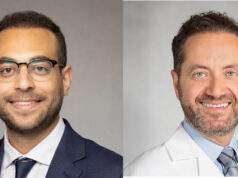
The research was presented today at both the 2025 VEITHsymposium in New York City (Nov. 18–22) by co-principal investigator Brajesh K. Lal, MD, a professor of surgery at the University of Maryland in Baltimore, and at the 2025 Society of Vascular and Interventional Neurology (SVIN) annual meeting in Orlando, Florida (Nov. 19–22) by James Meschia, MD, a vascular neurologist at the Mayo Clinic in Jacksonville, Florida. The trial has also been published in the New England Journal of Medicine.
CREST-2 was funded by the US National Institutes of Health (NIH), and is said to be the largest study to date comparing current treatment approaches for carotid artery disease caused by plaque buildup in the arteries supplying blood to the brain. According to the study researchers, although surgery and stenting have long been used to open these arteries, newer medications and better risk-factor control have raised questions about whether such procedures are still needed for people who do not have symptoms.
“Decades ago, surgery clearly helped prevent strokes in many patients,” said co-principal investigator and study senior author co-principal investigator Thomas Brott, MD, a professor of neurology from the Mayo Clinic in Jacksonville. “But medical therapy has improved so much that we needed to re-examine the balance between benefit and risk for people who have no symptoms.”
The CREST-2 program consisted of two parallel, randomized clinical trials conducted at 155 medical centers in five countries: Australia, Canada, Israel, Spain and the USA. Each of the trials enrolled more than 1,200 adults with severe carotid artery narrowing of 70% or greater who had not had a stroke or transient ischemic attack in the past six months.
In one trial, participants received either stenting plus intensive medical therapy or medical therapy alone, and, in the other, participants received endarterectomy plus medical therapy or medical therapy alone. All participants received comprehensive medical care—including lifestyle coaching and medication as needed—to manage their blood pressure, low-density lipoprotein (LDL) cholesterol and diabetes, and to help them stop smoking.
Researchers analyzed the occurrence of stroke and death within 44 days of stenting or surgery, and the occurrence of stroke over the course of four years on the same side of the body as the narrowed artery.
The trial comparing stenting versus medical therapy found a significant reduction in stroke; over four years, 2.8% of patients treated with stenting and medical therapy had a stroke compared to 6% of those on medical therapy alone—roughly halving the risk of stroke. However, in the endarterectomy trial, the difference in stroke rates—3.7% with surgery plus medical therapy versus 5.3% with medical therapy alone—was not statistically significant. In addition, serious complications were shown to be uncommon with either procedure.
The findings are believed to provide clearer guidance for physicians and patients considering a preventive procedure for carotid artery stenosis, with Brott emphasizing the importance of personalized decision-making as well.
“For some patients—particularly those with more advanced narrowing, or plaque that appears unstable or more likely to cause a blockage—stenting may offer added protection, while, for others, medical therapy alone may be enough,” he stated.
Close follow-up and coordinated care helped all participants in CREST-2 achieve and maintain significant improvements in their blood pressure and cholesterol levels, the researchers further claim.
Brott and colleagues will continue to track participants for long-term results, and they are also currently studying whether imaging tools can help identify which patients benefit most from each treatment.