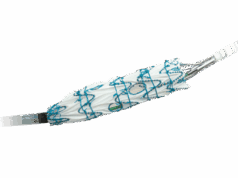
A novel physician-modified endograft (PMEG) technique for the treatment of thoracoabdominal and complex abdominal aortic aneurysms (TAAA and AAA) involving delayed-release diameter reduction to aortic size and shape—allowing for sequential target vessel cannulation—is safe and effective, according to a new study.
Results from the 203-patient analysis of PMEG fenestrated endovascular aneurysm repairs (FEVARs)—carried out in a physician-sponsored investigational device exemption (PS-IDE) at Dartmouth Hitchcock Medical Center in Lebanon, New Hampshire, from 2017–2024—were presented at the 2025 annual meeting of the New England Society for Vascular Surgery (NESVS) in Providence, Rhode Island (Sept. 26–28). Delivering the data, Kirthi Bellamkonda, MD, a vascular surgery resident at Dartmouth Hitchcock, set the scene: despite the emergence of commercial devices into the complex aortic aneurysm repair space, PMEG remains the predominant technology to treat these patients, and the traditional PMEG technique has changed little since its inception.
Bellamkonda reported an average aneurysm diameter of 59.9mm among the cohort, with a distribution of 24% juxtarenal aneurysms, 46% pararenal aneurysms, 10% extent IV TAAAs and 18% extent II or III TAAAs. Technical success was 100%, with 30-day outcomes showing 2.5% mortality, 2% organ failure (of which half was renal failure), about 1% paraplegia and paraparesis, and 5% access site complications.
At one year, there were no cases of open conversion, stent fracture or migration, Bellamkonda added. Paraplegia and paraparesis were found to be similar to the 30-day outcomes. One-year target vessel instability was 6.6%, of which 2% was component stenosis and 4.6% component occlusion.
So why delayed-release diameter reduction, Bellamkonda pondered. “We reduce the number of simultaneous wires from four to one compared to the traditional technique, which reduces the risk of wire loss and re-cannulation, as well as the trauma to bridge vessels,” she said. “This allows us to work with a smaller contralateral sheath and improves intraoperative efficiency.” Given the continued role for PMEG in complex treatment, Bellamkonda said that the study group hopes to see the technique and design disseminate and help inform industry improvements in graft manufacturing.