This advertorial is sponsored by Stryker/Inari Medical.
How a finely tuned stent surveillance program plays a crucial role in raising the alarm of worsening symptoms in DVT patients and identifies those who might require reintervention with mechanical thrombectomy.
For Jake Hemingway, MD, the key to his practice of treating patients with deep vein thrombosis (DVT) and the long-term effects in those who develop post-thrombotic syndrome (PTS) is not simply a robust, fastidious stent surveillance program, but something he thinks of as a wider DVT surveillance program.
The scope of the patient population is not insignificant, he says. “In a lot of hospital systems, patients with acute iliofemoral DVT get treated. People with superficial disease or varicose veins get treated. But there is a huge proportion of patients in between who have PTS or chronic sequelae of DVT that just aren’t really owned by anyone.”
Hemingway, an assistant professor of vascular surgery at the University of Washington (UW) in Seattle, is guided by a philosophy that includes a commitment to lifelong management and a program designed to capture patients with chronic venous disease of all segments who might otherwise fall through the cracks. He sees patients across the spectrum, but one population stands out: PTS patients who have undergone treatment at an outside facility and have had an early in-stent thrombosis, or those who have received a prior intervention that was ultimately unsuccessful. What unites them is the fact these patients tend to be younger and require long-term care.
“The reality is that nothing is permanent in vascular, so you really do have to deal with problems as they come up,” says Hemingway. So it stands to reason that, after placing a venous stent, “you should see that patient for life.” To that end, he continues, “it’s always easier to take care of a problem before it becomes a serious issue rather than dealing with a chronic occlusion many years later. Tied into that is that you need to understand what you’re doing to patients over the long term.”
Hemingway’s stent surveillance program is standardized. Follow-up appointments are scheduled at the same time as the index procedure. Patients receive an initial duplex ultrasound on postoperative day one. They are then followed at the two-to-four-week mark, after which—if their imaging is clear—they return at the three-, six-, and 12-month timepoints, then yearly thereafter. The surveillance program means issues that arise are picked up “much earlier on,” he adds.
When to re-intervene
Hemingway’s threshold for re-intervention is dependent on a couple of factors. “If a patient has a really challenging reconstruction and has a lot of inflow disease, and I think there might be something I can improve upon, I will look to go in,” Hemingway explains. “Or: if a patient comes in and they are outlining that they are not that symptomatic, but they missed a few days of anticoagulation, and now they have some in-stent thrombosis with an area that looks to be quite narrow and the flow is in continuous wave forms.”
He points to the classic case in point—in the setting of an inferior vena cava (IVC) and bilateral iliofemoral reconstruction. In these cases, the key to success is a combination of listening to the patient and treating recurrent symptoms.
To that end, the asymptomatic patient with a widely open stent will continue to be monitored under surveillance. But what about the patient who reports with either a 50%-or-more narrowing with associated flow abnormality like continuous waveforms peripherally? “We know there is a drop in the volume of flow rate in comparison to their postop day one duplex, especially if that is seen either at the two-week or three-month mark,” Hemingway says. “That’s when I’m much more aggressive about going in because I think you have your best chance of fixing things. With an early stent thrombosis, I will often have a lower threshold to intervene on a patient, especially if there is a narrowing that appears to be fairly significant and associated with more peripheral hemodynamic effects.”
Hemingway also re-intervenes when patients show evidence of stenosis and recurrent symptoms, whether mild or severe. “You see a change in the duplex, you notice some thrombus layering and continuous waveforms, with the patient noticing that their wound was healing well for two weeks, and now, over the last four weeks, it has stagnated or maybe even grown in size,” he explains. Then there are the patients with stents that appear to be clear but symptoms are recurring. “That’s when I start looking at superficial disease. I start to think about reflux, and other pathologies that might be contributing.”
All of which raises the question of treatment modality, and which cases point to which method of re-intervention. In most scenarios, Hemingway outlines, the most effective modality to remove in-stent thrombosis is mechanical thrombectomy with the RevCore thrombectomy catheter (Stryker/ Inari)—except in the setting of couple-of-weeks-old acute stent thrombosis.
“Unless I have a patient where I put a stent in, I have imaging that shows that it is open, and I have imaging that shows that it is occluded and I can definitively say that it is a two-week old-occlusion, then I’m generally likely to reach for the mechanical option because I think it does better with that sub-acute thrombus,” he says.
RevCore mechanical thrombectomy in action
Hemingway recalls a classic case using the RevCore Thrombectomy Catheter that underlines why the modality is his go-to in these types of scenarios.
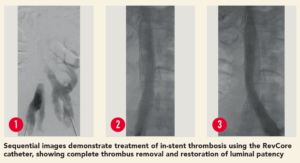 The patient was a 35-year-old male who presented with worsening back pain, leg swelling and edema that on imaging appeared to point to an acute DVT. Several years prior, he had undergone thrombectomy, IVC stenting and a bilateral iliocaval reconstruction for chronic IVC occlusion and associated iliofemoral thrombosis. The IVC and common iliac vein (CIV) stents were thrombosed.
The patient was a 35-year-old male who presented with worsening back pain, leg swelling and edema that on imaging appeared to point to an acute DVT. Several years prior, he had undergone thrombectomy, IVC stenting and a bilateral iliocaval reconstruction for chronic IVC occlusion and associated iliofemoral thrombosis. The IVC and common iliac vein (CIV) stents were thrombosed.
“Both sides had gone down,” Hemingway explains. “One was thrombosed all the way through, the other had a wisp of flow going through it. I took the patient for a venogram and tried aspiration without success, so then tried the RevCore. What we got out was all white, rubberish, fibrotic material. This is someone in whom, had I opted for aspiration thrombectomy, I would have had to reline the whole stent reconstruction. We were able to clean out the stent and send the patient home without any new stents being placed.”
Post-intervention, the patient was noted to have brisk flow on venogram, no thrombus layering on intravascular ultrasound (IVUS), and no further stenting was required. Now 18-months post-procedure, the patient has sustained full patency and complete symptom resolution.
Decisions around intervention are influenced by timing, Hemingway points out. “If a patient has an occluded stent for six months or longer, I think that the results are less predictable and it is a little harder to know whether you’re going to get great thrombus clearance,” he says. “If it is a case of less than six months and definitely less than three months, my experience has been that RevCore has worked very well for clearing out in-stent thrombosis. If you are patient, and really work the areas, you use the device correctly and really grind away at that thrombus layer by layer, you will get it cleared out. Once it gets to be rock hard or associated with calcification, there’s just some pathology you can’t pull out of there.”
This is an article sponsored by Inari Medical. The HCPs sharing their views and opinions here express their experience with Inari Medical devices. The HCPs’ opinions of these devices were formed independently of Inari Medical and may not represent every experience or outcome with the devices.
Indications For Use: The RevCore thrombectomy catheter is indicated for (1) the non-surgical removal of thrombi and emboli from blood vessels and (2) injection, infusion, and/or aspiration of contrast media and other fluids into or from a blood vessel. The RevCore thrombectomy catheter is intended for use in the peripheral vasculature. Review complete Instructions for Use, Indications for Use, Warnings, Precautions, Possible Adverse Effects and Contraindications prior to use of the product.
Caution: Federal (USA) law restricts this device to sale by or on the order of a physician. For all non-Inari products, please refer to complete manufacturer Instructions for Use/Intended Purpose. All copyrights and trademarks are the property of their respective owners. PRO-2406-USA-EN-v1